I needed awhile to process the “first date” that I endured with the specialist before I wrote a blog post. It didn’t go as I had hoped, and as “first dates” are concerned this wasn’t the best one I have sat through. So yesterday, I cleaned and organized while I thought about what I took away from that experience. I spent my day boxing up the old, and throwing away objects that no longer please or serve me. I don’t need a trip to the psychologist to figure out that this new energy to purge was a manifestation of “sorting” through this frustrating journey of heart failure: one that has seemingly endless curves and detours. A journey that has taken me away from my life, or at least the one I would like to live.
My husband and I traveled a couple hours to visit the transplant center within a huge hospital. We arrived; waited; was moved around to various compartmentalized areas; waited some more; had a chest x-ray, and then was ushered into a small, dark room. (The entire day at the center was 6 hours – and an additional 4 hours of driving). We sat in this room almost 3 hours before the doctor arrived. We were anxious and perturbed that we had to wait for so long. I came prepared with a large file of all the medical records for the last 8 years that I had in my possession. I gave his assistant a copy of that file 3 hours before, when we were first brought in. We had thought maybe he was reviewing the file before he saw us, which would explain the long wait, but that belief was quickly dispelled once he started asking questions – all of which he could have found the answers to in the file I provided him. Of course, instead of just answering him, I told him where he could find that information in the file. I came prepared; he should have been also. So the first impression wasn’t very impressive.
The initial consultation started very awkwardly, and by the doctor saying, “doing nothing, and not making you miserable while you live out the rest of what life you have left, is sometimes the best method of treatment.” Ummm…WTF? Glad I spent years of expensive and painful tests just to get to a “heart failure specialist!” Well, Gee! I just live incapacitated until I die of it? Thanks for your well-educated and respected opinion! Maybe this was just a “knee-jerk” response from him, to someone that he couldn’t easily diagnose? I really don’t know. I am still grappling with an explanation; especially seeming how he hadn’t even started treatment with me yet. Look, I am ALL for “pushing me down river” if all hope is lost and in an effort to not make me suffer through treatments that prolong my life miserably, if not only shortly. But this guy puts out the disclaimer at the gate! Most cardiologists I have been to, take at least a year until they give up. Disappointment bottomed-out at that moment in an environment that felt much like my future with heart failure: dank, prison-like, airless, and formidable. My hope of finally having a resolution looked bleak. **On a side note, as a designer who is especially interested in healthcare environments, this hospital is the most depressing hospital I have ever walked through – maybe I should leave my business card.
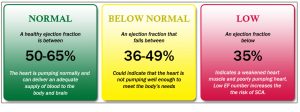
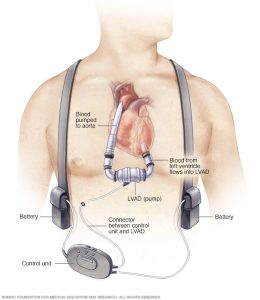
The conversation waxed-and-waned through what other causes that hadn’t been explored too much by previous cardiologists, such as neurological issues of “nerves not talking to my heart” and exploring my moderate sleep apnea some more. I am sure there must be a “method to his madness” in revisiting the sleep study, but more likely, some grasping in the dark happening…again. I will give this guy the same shot to figure it out, just like the last guys, but I cant help like feeling, at least initially, that this is just more dancing, but by a different clown. I expected more from a specialist, I guess. I am told by loved ones to give him a chance; that he is new to my issues. I understand that. But I am NOT new to this issue and I am ready (desperate, really) for someone to tell me, “I got you.” I don’t believe it will be this guy. I will say that the “something good” I walked away with, is that he is exploring other ways outside of heart transplant to fix my heart ailment, and that was definitely something I had wanted him to do. However, if the problem ends up being a neurological one, he wouldn’t discuss how that problem would be fixed, saying, “we will discuss that when we get to it.” So, I am not sure all this circling will not just bring us right back to heart transplant in the future. Next week I start his regime of additional testing and hopefully a direction will be pursued.
He reiterated the difficulty of my case, over and over, and even called me an “outlier.” Ok, ok, it is hard, but that is why I am here! You are the expert! Can you, or can you not, fix me? I had my answer about an hour into our appointment; if he cannot, he will refer me to the “big guns” at Mayo Clinic in Rochester. There we go…his out, even before we actually begin.

I feel deflated by this appointment, not buoyed as I had hoped. I know that tomorrow is another day, and the fight will start anew; but today I am tired. Tired of meeting up to that fight to be told that the enemy is not who we thought, unrecognizable, and, therefore, unbeatable. So today, I will take a much needed rest in this journey, and follow his first “knee-jerk” advice (or maybe just plain “jerkish” advice) and do just as he stated: nothing.